Consuming alcohol can provide a welcome reprieve from the hassles of every-day life but can lead to binge drinking and excessive alcohol consumption. Over time, too much alcohol use results in developing chronic diseases and other serious problems.
UCLA scientist and pathologist Dr. Samuel French published a review on the effects of chronic alcohol binging on cell health. In his review, Dr. French examined how binge drinking causes injury to the liver and other organs by diminishing the cellular levels of the molecule nicotinamide adenine dinucleotide (NAD+).
NAD+ is a coenzyme—a compound necessary for the functions of proteins called enzymes—in numerous metabolic reactions critical for healthy aging, like the generation of cellular energy (i.e., reduction-oxidation reactions). NAD+ binds to enzymes called sirtuins to promote cellular health through DNA repair.
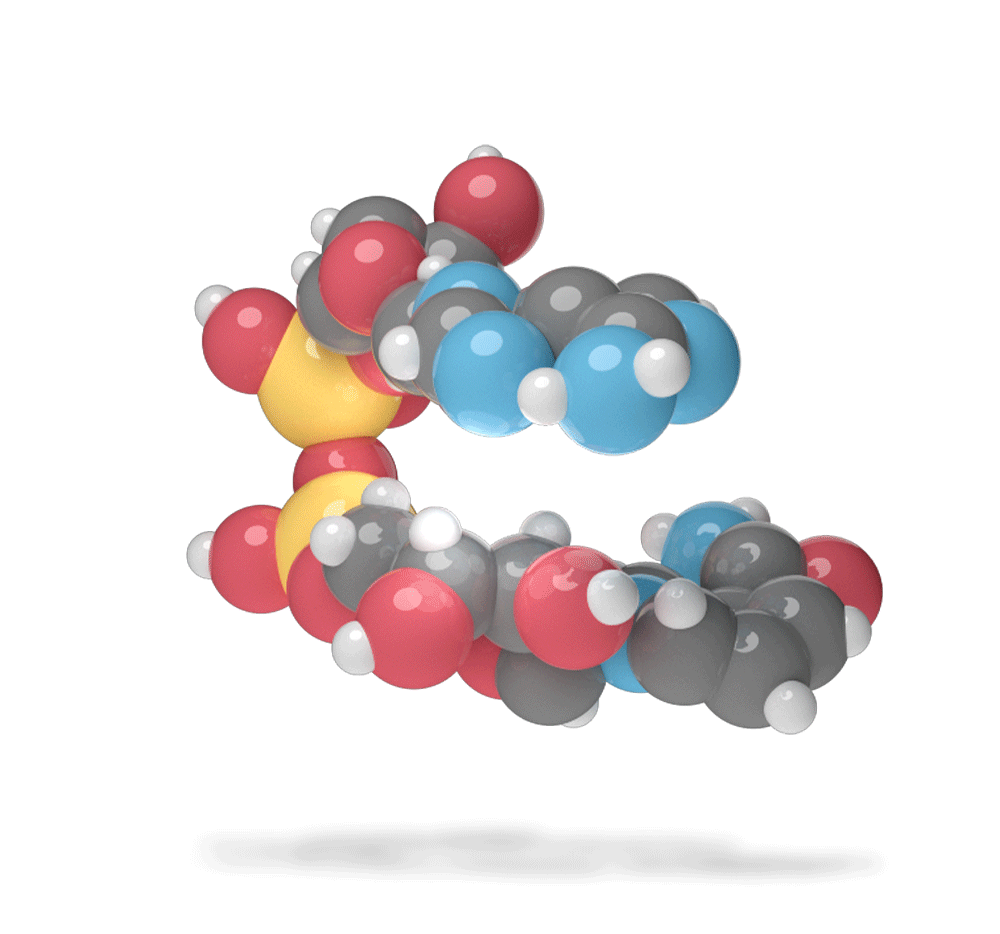
Dr. French’s review highlights studies that show high blood alcohol levels result in the conversion of NAD+ to the molecule NADH that inhibits its ability to perform its functions as a coenzyme. With high blood alcohol levels, sirtuin enzymes also become more abundant in cells. However, with diminished NAD+ levels to facilitate sirtuin function, there is an elevated amount of protein changes in liver cells that induce inflammation and, ultimately, cause alcoholic fatty liver disease. What’s more, all enzymatic activities that depend on NAD+ shut down, leading to reduced lifespan.
The review also covers studies showing that diminished NAD+ availability alters the body’s 24-hour clock (i.e., circadian rhythm), which can negatively impact metabolism and energy generation from the cell’s powerhouse, the mitochondria. Reduced NAD+ concentrations affect the body’s circadian rhythm by disrupting sirtuin activity that modulates proteins critical to maintaining the body’s clock.
“NAD is a linchpin of energy metabolism and its diminishing level with age has been implicated in mitochondrial deterioration during aging,” concluded Dr. French. Long term alcohol use and binge drinking can contribute to these effects by reducing NAD+ levels and facilitating the dysfunction of sirtuins and mitochondria. The review suggests that boosting NAD+ levels can increase sirtuin activity for beneficial cellular effects, like the generation of new mitochondria. Along these lines, research has shown that NAD+ boosters like nicotinamide riboside (NR) and nicotinamide mononucleotide (NMN) can prevent mitochondrial deterioration.