Our sleep quality influences not only our energy levels but also our hunger intensity. It follows that, while good sleep can give us the energy to exercise, poor sleep may make us feel unmotivated. While good sleep can make us feel satiated, bad sleep can make us feel hungry and prone to overeating. Thus, good quality sleep lies the foundation for consistent exercise and food intake routines, together comprising the three pillars of health and longevity.
What is good quality sleep? The most well-known indicator of good quality sleep is sleep duration — about 7 to 9 hours is recommended. However, sleep duration alone fails to tell the whole story. As reported in Progress in Cardiovascular Diseases, Baranwal and colleagues from Brown University review the latest sleep science research while Figueiro and Pedler review the latest circadian rhythm research, which is summarized here.
Importance of Sleep
Stages of Sleep: The Need for Deep and REM Sleep
It wasn’t until 1953 that American scientists Nathaniel Kleitman and Eugene Aserinsky discovered that sleep is comprised of different stages. Each stage is characterized by distinct brain wave frequencies, measured by an electroencephalogram (EEG).
Without measuring our brain waves, it is difficult to know if we are getting sufficient levels of sleep. Still, sleep quality can be estimated based on our movements, which is how sleep trackers assess sleep quality. We can also personally assess our sleep quality by how energized we feel upon waking.
There are four stages of sleep, three stages of non-rapid eye movement (NREM) sleep and a fourth stage of rapid eye movement (REM) sleep. Good sleep encompasses 4-5 cycles of all four stages, each cycle lasting about 90 minutes. After REM sleep, a bout of wakefulness may occur before repeating the cycle again.
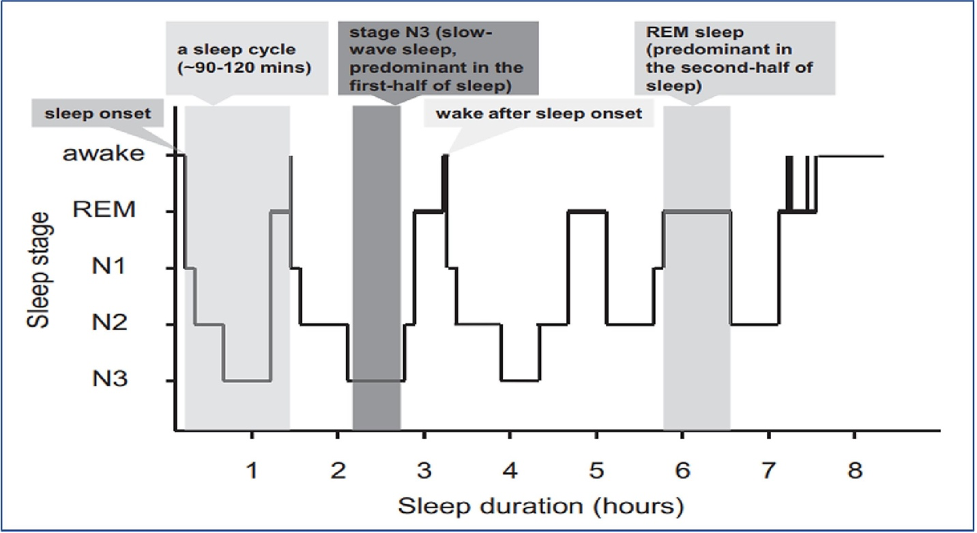
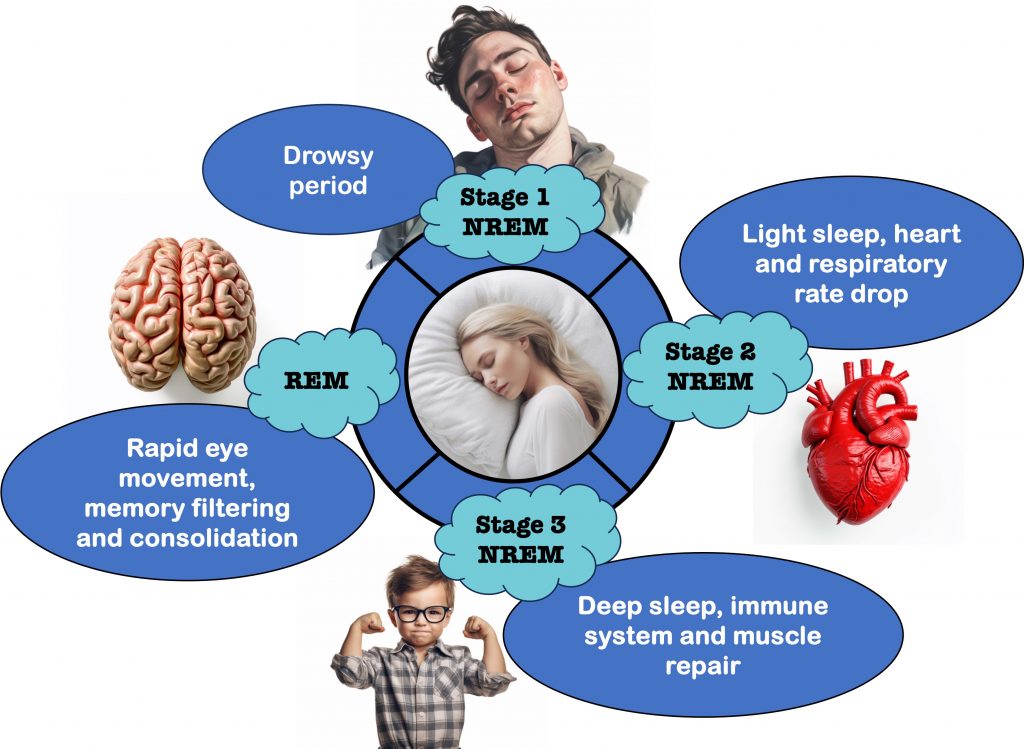
As we ascend into sleep, we enter a drowsy period known as Stage 1 NREM sleep, the lightest stage of sleep. Stage 2 NREM sleep is a slightly deeper level of sleep, whereby our heart rate and breathing begins to slowdown.
Stage 3 NREM sleep is the deepest level of sleep, characterized by slow-brain waves called delta waves. During this stage, our immune system is strengthened while our muscle is repaired, allowing for growth and strengthening.
REM sleep is critical for memory consolidation — storing memories for long-term access. This consolidation process includes a filtering process, whereby unimportant memories aren’t consolidated. This process requires neuroplasticity — the process of strengthening the connections between neurons in the brain to learn information.
During REM sleep we are unable to move due to muscle paralysis. Since REM sleep is also when we dream, this inability to move protects us against acting out our dreams, which could be dangerous.
Circadian Rhythm-Aligned Sleep Promotes General Health
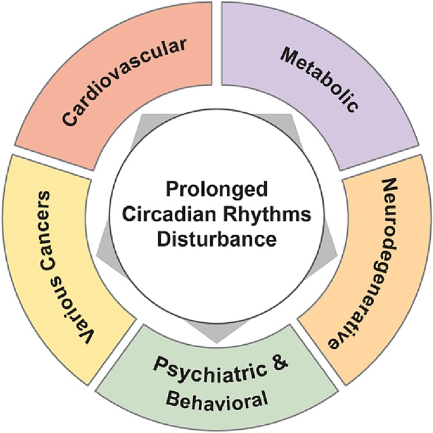
Research from the past 40 years has established a clear link between circadian rhythms and general health. Circadian rhythms are the physiological oscillations that occur over 24-hour cycles, modulating everything from when we feel sleepy to when we feel hungry.
Our circadian rhythms synchronize our internal physiological processes with the external environment, which is largely set by light entering the eye. The desynchronization of our circadian rhythms with our external environment is associated with several chronic diseases.
The physiological processes controlled by our circadian rhythms are synchronized by a structure in the brain called the suprachiasmatic nucleus, or the “master clock.” The master clock times our drive to be awake, called the alerting force. This alerting force opposes our drive to sleep.
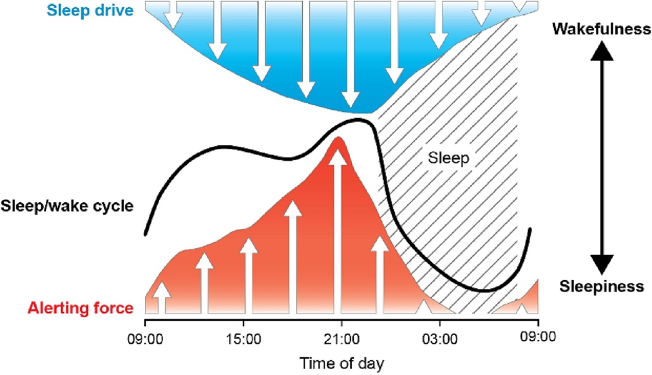
Circadian rhythms also control the release of hormones like melatonin and cortisol. Melatonin is secreted upon darkness and promotes sleepiness while cortisol is released upon waking. Although cortisol is known as the stress hormone, it is important for cardiovascular, metabolic, and brain health.
Our master clock is on a slightly longer cycle than 24-hours, which over time can lead to asynchrony with the environment. Still, the master clock can be reset by various environmental cues, especially sunlight.
Other less powerful cues include the timing of meals (but not eating itself), exercise, and social activity. This means that if our circadian rhythms become disrupted, there are ways to put them back on track (see below).
Good Sleep Counters Death and Disease
Poor sleep includes not getting enough sleep, sleeping for too long, disrupted sleep stages, and sleep disorders like insomnia and sleep apnea. Poor sleep can disrupt the body’s repair systems and lead to a host of health problems, including those related to hormones, the cardiovascular system, the immune system, and the brain. Furthermore, poor sleep, as measured by sleep duration, is a predictor of early all-cause mortality.
Lifespan
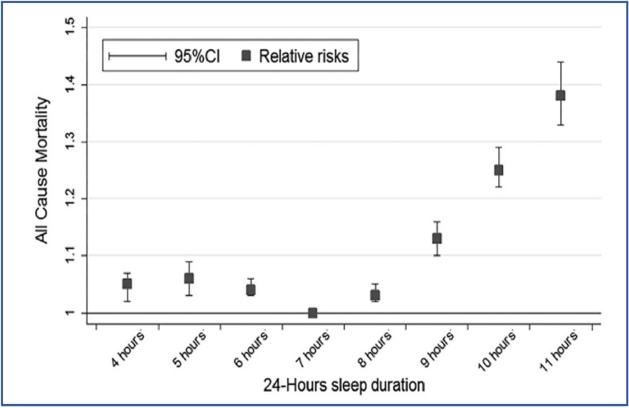
In one of the largest analyses of its kind, 40 studies were combined to include over 2 million participants. The purpose of the analysis was to determine the association between sleep duration and all-cause mortality. It was found that, compared to a 7-hour sleep duration, both shortened and prolonged sleep duration was associated with increased risk of all-cause mortality.
Animal studies have more directly shown that poor sleep, specifically sleep deprivation shortens lifespan. For example, Harvard scientists have shown that sleep deprivation shortens the lifespan of fruit flies by 50% due to reactive oxygen species (ROS) in the gut. ROS are normally neutralized by cellular antioxidants but can accumulate during aging, or in this case sleep deprivation, suggesting that poor sleep accelerates aging.
Hormones
Our hormones are like master regulators of our entire body. When our hormones become dysregulated, it can negatively affect all of our cells.
Studies show that poor sleep induces impairments to the hormone insulin, promoting high blood glucose levels and inflammation, eventually leading to type 2 diabetes. Thus, good sleep can deter the chances of succumbing to diabetes.
Poor sleep suppresses the hormone testosterone, potentially triggering sexual dysfunction. Additionally, disruptions in growth hormone can deter muscle growth and repair, possibly increasing the risk of muscle atrophy.
Furthermore, poor sleep-induced alterations in the balance between ghrelin (the “hunger hormone”) and leptin (the satiety-related hormone) may increase hunger during waking hours, increasing the risk of obesity.
Cardiovascular System
Sleep gives our heart a chance to rest, as during normal sleep, our heart rate slows, and our blood pressure drops. Poor sleep is associated with an increased risk of coronary artery disease, stroke, and heart attack.
Immune System
Poor sleep can increase illness susceptibility by weakening the immune system.
Studies show that poor sleep reduces immune cells called natural killer cells (NKCs), which not only fight off infections but also kill cancer cells. This means that poor sleep could increase the risk of cancer.
Furthermore, a weak immune system can increase inflammation. Chronic low-grade inflammation is thought to drive the aging process and may contribute to conditions like neurodegeneration.
The Brain, Memory, and Mental Health
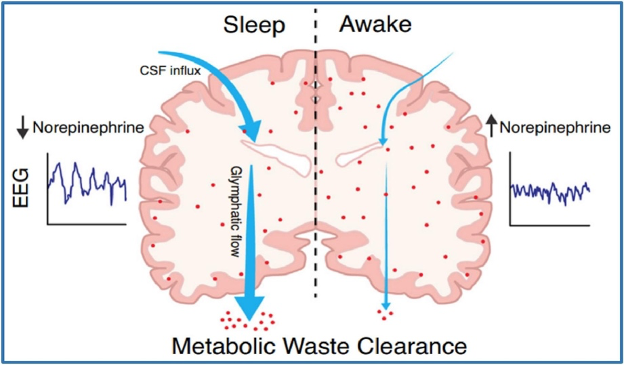
When awake, our brain accumulates waste products, which are cleared from the brain during sleep. These waste products can potentially include amyloid, a protein associated with Alzheimer’s dementia. Thus, poor sleep is associated with an increased risk of Alzheimer’s, other neurodegenerative disorders, and cognitive impairment.
Individuals with depression may suffer from insomnia and poor sleep, while insomnia and poor sleep can lead to depression. Insomnia and poor sleep also increase the risk of anxiety, addiction, and poor mental health. Additionally, a lack of good sleep in the short term may lead to irritability, fatigue, and challenges with focusing.
Optimizing Sleep and Circadian Rhythms For Longevity
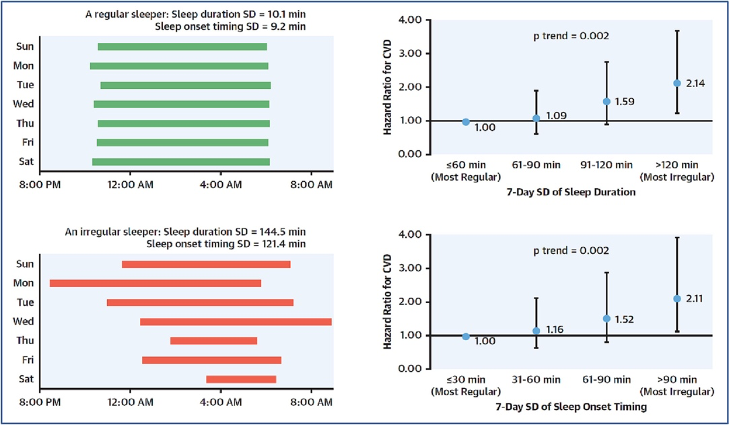
Sleep hygiene refers to behavioral and lifestyle interventions that promote better sleep quality and duration. In addition to getting 7 to 9 hours of sleep, a consistent sleep schedule may be the most important aspect of sleep hygiene.
This is highlighted by a study showing that an irregular sleep schedule increases the risk of fatal or non-fatal cardiovascular complications. A consistent sleep schedule involves simply going to sleep and waking up at the same time every day.
Exercise and Weight Loss
Exercise has long been known to improve sleep quality. The American Heart Association recommends 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity exercise to achieve the benefits of improved sleep from exercise. A 30-minute exercise session can also improve sleep quality that same night.
Another benefit of exercise is weight loss. Optimal body weight can also improve sleep quality, largely due to reducing sleep-disordered breathing in individuals with sleep apnea. Overweight individuals are also more likely to suffer from gastroesophageal reflux disease (GERD), which can result in waking up during the night due to discomfort.
Limiting Caffeine, Alcohol, and Late-Night Unhealthy Meals
Studies have shown that caffeine reduces Stage 3 NREM deep sleep, increases Stage 1 NREM shallow sleep, and promotes waking during the night. The effects of caffeine dwindle 6-7 hours after consumption, so caffeine intake should ideally be stopped about 6 to 7 hours before sleep.
As a sedative, alcohol may help with falling asleep, but it also reduces REM sleep duration and overall sleep duration, resulting in poor sleep quality.
Avoiding food intake at least two hours before sleep is advised to improve sleep quality. Eating too late is associated with poor sleep quality and weight gain. However, many individuals consume less healthy foods before sleeping.
Poor sleep quality from eating food close to bedtime may be mitigated by only eating nutrient-dense, low-energy, and/or single-macronutrient foods. For example, a small portion of yogurt, or an orange.
Bedtime Environment and Mindset
A dark, cool, and quiet sleep environment is recommended for good sleep quality. A cooler sleep environment is associated with deeper sleep. It is also advised to use one’s bed only for sleep and not work, studying, watching videos, etc.
Additionally, mindfulness may improve sleep quality, especially for those with insomnia. Mindfulness practice may also be helpful for those who ruminate and think a lot before sleep. Mindfulness involves quieting the mind by focusing on the breath, just observing your thoughts, or focusing on other things like sensations of the body.
Circadian Rhythm Alignment
Our circadian rhythms have a profound influence on our sleeping habits. Therefore, to optimize sleep, our circadian rhythms should be aligned with the state of our environment. Since we are not nocturnal, our sleeping hours should be during the night if possible. Additionally, waking up and going to sleep at the same time every day helps with both sleep hygiene and circadian rhythm alignment.
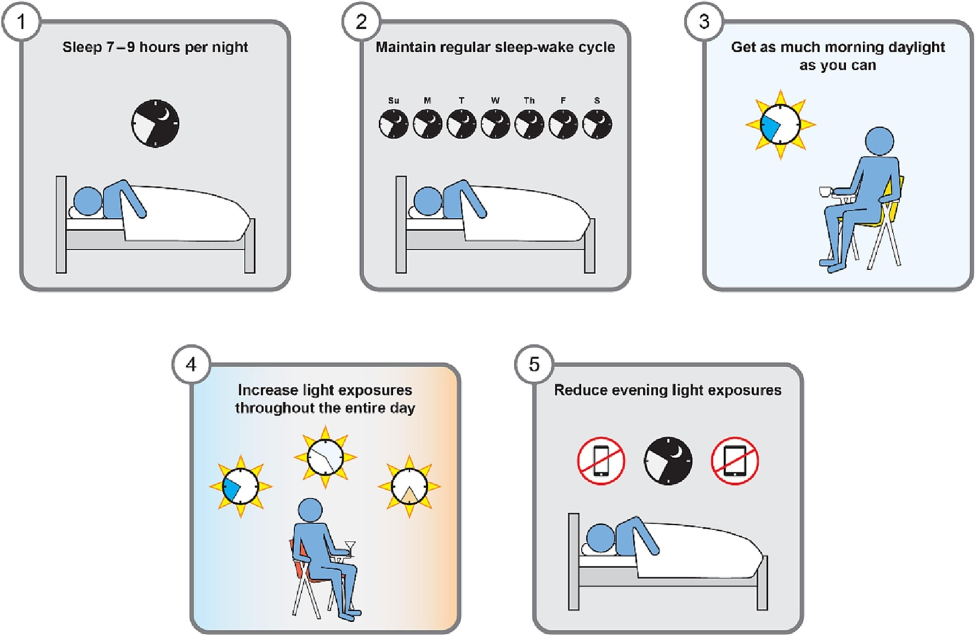
Our circadian rhythms are entrained by light, so getting sunlight as soon as possible after waking is recommended. Doing this at around the same time each day will help with regular sleeping patterns, as early sunlight determines when melatonin will be released later in the day.
Increasing exposure to sunlight throughout the day also helps to align internal biological clocks with the state of the environment. Getting sunlight throughout the day is like telling your body it’s daytime.
As light promotes wakefulness, darkness promotes sleepiness. Therefore, reducing light exposure after the sun has gone down will help with circadian alignment. It is recommended to reduce light exposure about two hours before bedtime.
Reducing light exposure can be accomplished by dimming the lights and avoiding luminous screens if possible. Otherwise, the screen brightness of televisions, smartphones, electronic notebooks, etc. can be dimmed.