Many studies over the last few decades support the notion that declining function of the cell’s power-generating structure, the mitochondria, is linked with obesity, insulin resistance, and type 2 diabetes for rodent and human tissues. Studies have also shown metabolic impairments that come from diminished levels of a molecule called nicotinamide adenine dinucleotide (NAD+) that has essential roles in cellular energy production and maintenance of cell health in these diseases. Lifestyle choice changes, like exercise and calorie intake reductions, remain the best choices for mitochondrial health improvement in people to fight against these metabolic diseases. However, some researchers have considered the possibility that supplementing with an NAD+ precursor called nicotinamide riboside (NR) could mitigate the severity of these diseases as well.
A commentary by Moore and Mucinski from the Harry S. Truman Memorial Veterans Medical Centre in Missouri published in The Journal of Physiology looked at a clinical trial performed by Dollerup et al. (2020) that did not give evidence for the proposal that NR supplementation improves NAD+ content and mitochondrial function in human skeletal muscle. Their commentary discussed how the findings obtained in the study by Dollerup and colleagues run counter to the prevailing idea that NR supplementation increases NAD+ levels and improves mitochondrial function in humans.
Researchers have sought to target NAD+ therapeutically for increasing its abundance in cells with the B3 vitamin NR. Studies have shown that NR increases NAD+ levels in rodent blood and tissue, leading to increased NAD+ bioavailability–the amount of NAD+ that is active when introduced to the body–and protection from insulin resistance and obesity in mice fed high-fat diets. Recent data has also shown that NR supplementation improves NAD+ bioavailability and is well-tolerated in people, but it has remained unclear whether NR supplementation enhances insulin resistance and mitochondrial function.
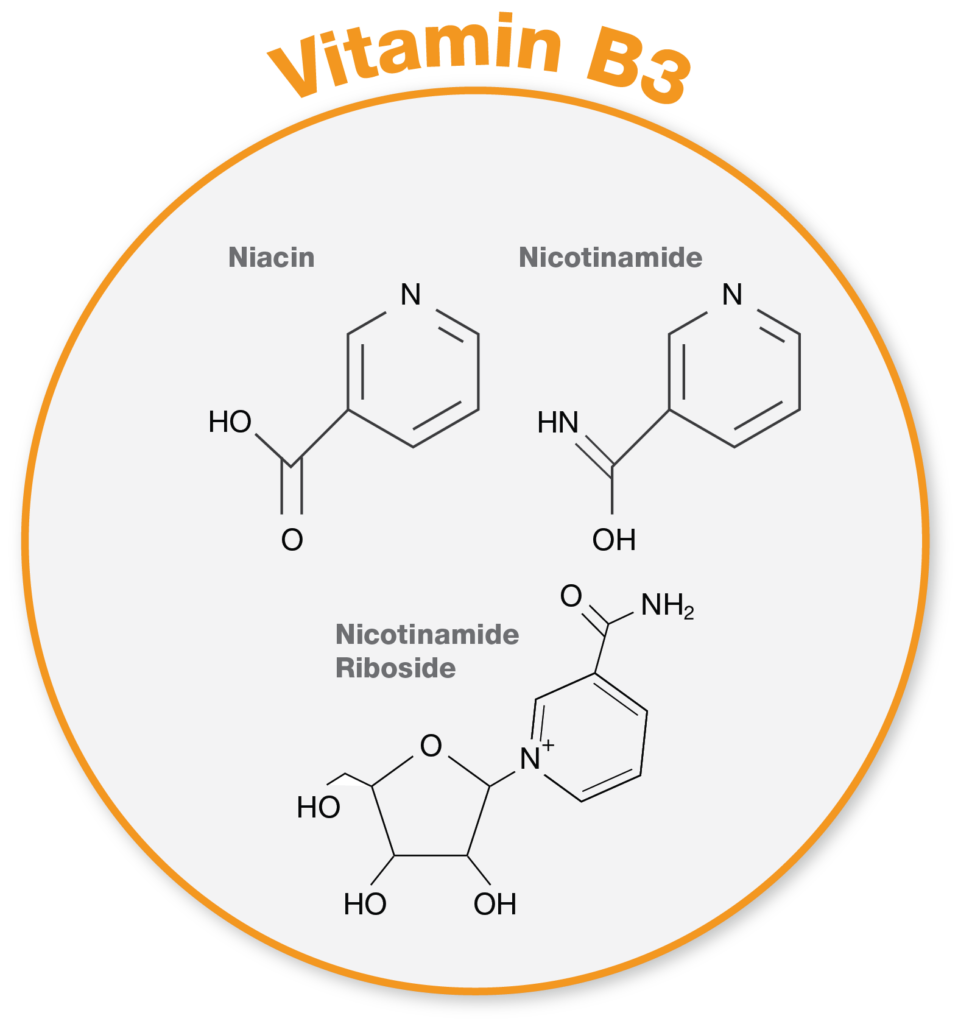
Vitamin B3. Vitamin B3 complex includes three forms: nicotinamide, niacin, nicotinamide riboside.
The recently-published study investigated NR supplementation effects for 12 weeks of treatment to see whether administering NR is safe and improves insulin sensitivity and the function of mitochondria. The team of researchers supplemented 1,000 mg of NR twice daily to obese males from a cohort of 40 men randomized to receive NR or placebo for 12 weeks. This report published in The Journal of Physiology also evaluated the effects of supplementing with NR on the content of mitochondria in skeletal muscle, respiration (a measure of oxygen consumption indicative of metabolism), and mitochondrial shape in obese men.
The study’s data challenge the current thinking that supplementation with an NAD+ precursor like NR enhances human skeletal muscle mitochondrial function. These results align instead with another recently-published study from Elhassan et al. (2019) demonstrating that NR supplementation in a small cohort of aged men from 70-80 years old did not affect metabolism. The data from the Elhassan and colleagues study indicated no NAD+ level or skeletal muscle mitochondrial function changes, which does not fit with the data from supplementing rodents with NR. “The studies from Dollerup et al. indicate that further scientific evidence is required before recommending the use of NR supplementation or other NAD+ precursors,” stated Moore and Mucinski in their article.
Although the data do not support current thinking that NR enhances the structure and function of mitochondria in human skeletal muscle, the study only included obese middle-aged males with insulin resistance. Future studies could examine whether NR supplementation significantly affects populations of different age, sex, and more severe metabolic diseases like type 2 diabetes. There is also the possibility that NR supplementation improves NAD+ content and mitochondrial function in specific human tissues other than skeletal muscle, like fat, liver, or immune cells. Different tissues could have distinct NAD+ level bioavailability, and the possibility remains that human skeletal muscle has low bioavailability.
“It would also be interesting to explore whether other supplementation strategies aimed at boosting NAD+ metabolism, such as nicotinamide mononucleotide [NMN], have differing effects compared to NR supplementation,” said the authors of the article. Maybe NMN, another NAD+ precursor, affects NAD+ bioavailability differently in human skeletal muscle. Clinical trials investigating the NMN supplementation’s effects in humans are underway and could provide further revelations into this matter.