Key Points
- A metabolite analysis in human kidney tissue shows that nicotinamide adenine dinucleotide (NAD+) deficiency is strongly associated with kidney disease.
- NAD+ deficiency is associated with kidney disease in a mouse model, also.
- NMN and NR treatments restore NAD+ levels and improve markers of kidney function without significant treatment differences in a male mouse model of kidney disease.
Research has already shown that treating mouse models of kidney disease with NAD+ precursors like NMN prevents kidney damage and improves kidney function. However, no direct comparison between the efficacy of NMN and another potent NAD+ precursor – NR – have been performed until now. NR must be converted to NMN before transforming to NAD+, so some have questioned whether these pathway differences lead to discrepancies in their capabilities to ward off age-related diseases like kidney disease.
Published in Nature Metabolism, Susztak and colleagues from the University of Pennsylvania show that NMN and NR alleviate kidney disease in a male mouse model without significant differences in their efficacies. Through metabolite analyses, their data show NAD+ deficiencies occur in both humans and mice with kidney disease. The research team goes on to demonstrate that NMN and NR reduce two molecular markers of kidney dysfunction – creatinine and blood urea nitrogen (BUN) – to similar degrees in a mouse model. These findings suggest that, at least in the case of kidney disease, NMN and NR confer similar beneficial effects.
NAD+ Deficiency Underlies Kidney Disease
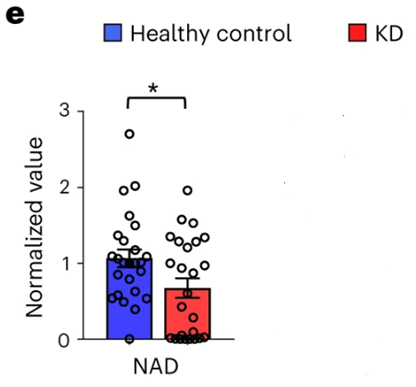
To get a better grasp on the underlying molecular pathways contributing to kidney disease, Susztak and colleagues analyzed kidney tissue metabolites in older humans with kidney disease. Their metabolite analysis revealed two primary metabolites with altered levels in kidney disease – nicotinate and nicotinamide. These metabolites are key players in NAD+ metabolism, so the researchers measured NAD+ levels in the kidney disease patients and compared them to healthy adults. They found that NAD+ levels were significantly reduced in adults with kidney disease.
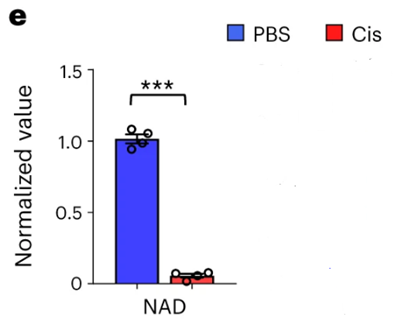
The research team wanted to mimic kidney disease in mice and be sure that their model exhibited the same underlying pathology as humans – NAD+ deficiency. Susztak and colleagues induced kidney disease by injecting the chemotherapeutic agent cisplatin into the mice. Similar to what was found in humans with kidney disease, the Pennsylvania-based team found significantly reduced NAD+ levels in the kidneys of cisplatin-treated mice. These findings suggest that NAD+ deficiency is present in this model.
Susztak and colleagues treated kidney disease mice with NMN or NR to compare their efficacies. They found that NMN and NR significantly reduced levels of two molecular markers for kidney dysfunction – creatinine and BUN. The researchers found no difference between NMN’s and NR’s effects on these kidney dysfunction markers. These results suggest that NMN and NR give similar benefits to ameliorate kidney disease in a mouse model.
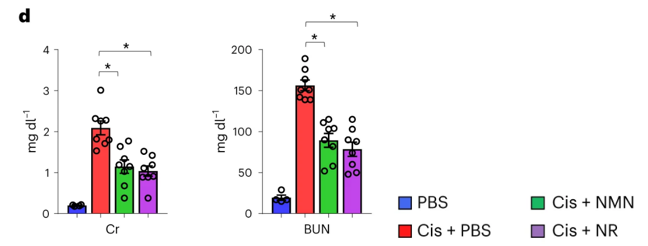
“The effectiveness of NMN and NR has rarely been compared head-to-head, but our results show that they have similar protective effects and drive comparable restoration of renal NAD+ levels in kidney disease models,” said Susztak and colleagues.
Directly Comparing NMN and NR in Other Organ Systems and Diseases
The study is one of the first to directly compare NMN and NR, and it shows that the two molecules relieve markers of kidney disease with similar degrees of benefit in a mouse model. Both NMN and NR have been found to increase blood NAD+ levels in humans and rodents, so both molecules target a proposed underlying pathology of kidney disease – NAD+ deficiency. More studies using organ systems like the liver, skeletal muscle, and cardiovascular system must be employed to directly compare NMN and NR’s effects. Such studies will pave the way to finding which of the two molecules is superior in particular organ systems and disease contexts.