Boosting nicotinamide adenine dinucleotide (NAD+) levels with precursors like nicotinamide riboside (NR) has become popular as a means to fight off age-related diseases that come from dysfunction of the cell’s powerhouse, the mitochondria. Human studies evaluating NR supplementation’s effects have sought to determine whether NR can in fact alleviate and prevent these diseases.
Past studies have shown that supplementing rodents with NAD+ precursors like NR stimulates metabolism by enhancing the production of mitochondria in skeletal muscle, but oral NR administration has only been shown to raise human NAD+ levels in the blood. Researchers from Denmark published a study in the Journal of Physiology where they tested long-term (12 week) NR supplementation and its effects on NAD+ content and mitochondrial function in human skeletal muscle. The research team found that supplementing with NR doesn’t increase skeletal muscle NAD+ levels or mitochondrial function in obese and insulin-resistant men, suggesting that NR supplementation’s effects in rodents will not translate to humans.
Healthy metabolism depends on mitochondrial function, which deteriorates progressively as a result of age-related reductions of NAD+ levels in mice and human tissue. Studies have linked these declining NAD+ levels with age-associated diseases like obesity, insulin resistance, and type 2 diabetes, which result in dysfunctional metabolism regulation in skeletal muscle. Past studies have shown that the naturally-occurring vitamin B3, NR, increases NAD+ levels in mice to stimulate cellular reactions that generate energy and promote cell health maintenance.
For these reasons, the Denmark-based team of researchers examined human tissue skeletal muscle to find out whether NR supplementation increases human NAD+ levels and improves mitochondrial function. Their study included 40 participants that received 1000 mg of NR or placebo twice daily for 12 weeks. The study didn’t show that NR improves NAD+ levels in the skeletal muscle of men with obesity and insulin resistance.
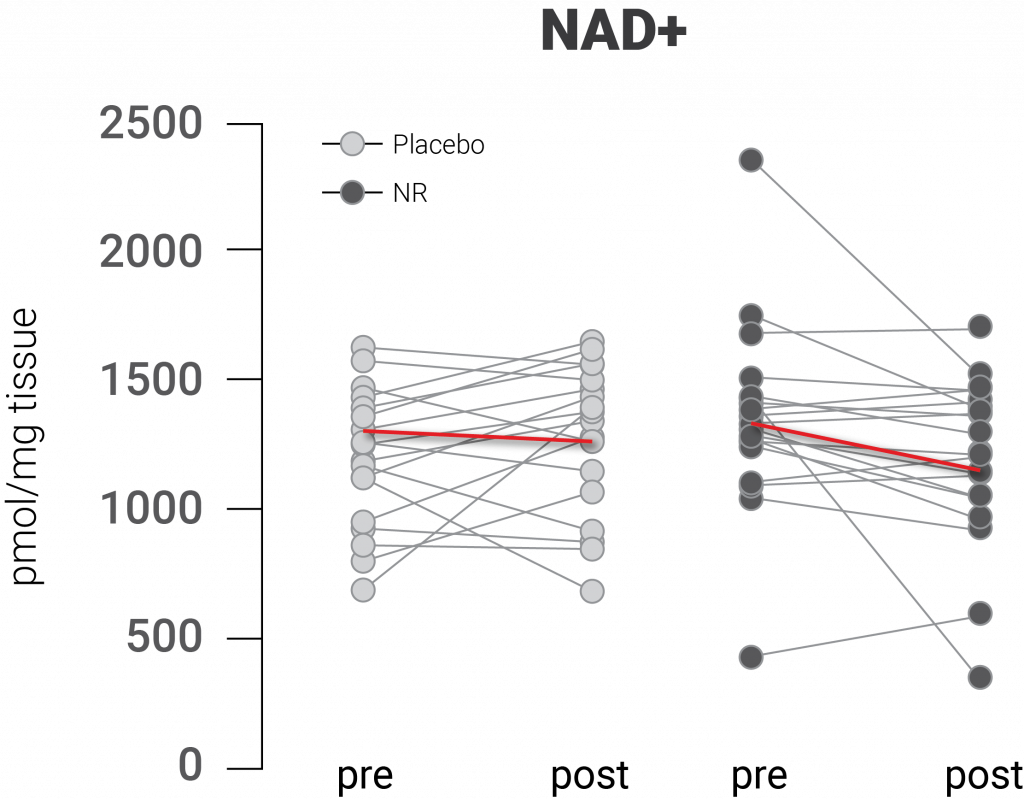
(Dollerup et al., 2020 | Journal of Physiology) NR supplementation does not increase NAD+ levels in human skeletal muscle. The figure indicates no differences in NAD+ levels before and after placebo and before and after 12 weeks of NR supplementation.
The researchers found that NR supplementation did not affect the abundance of skeletal muscle mitochondria, either. Since past studies have demonstrated that NR treatment induces mitochondrial production in skeletal muscle cells of rodents, the research team wanted to find out whether these same effects happen in people. To do so, they measured mitochondrial protein levels after 12 weeks of NR supplementation but found no noticeable differences. They also measured the levels of citrate synthase, an enzyme with activity that correlates with mitochondrial abundance, and found no effect from NR supplementation.
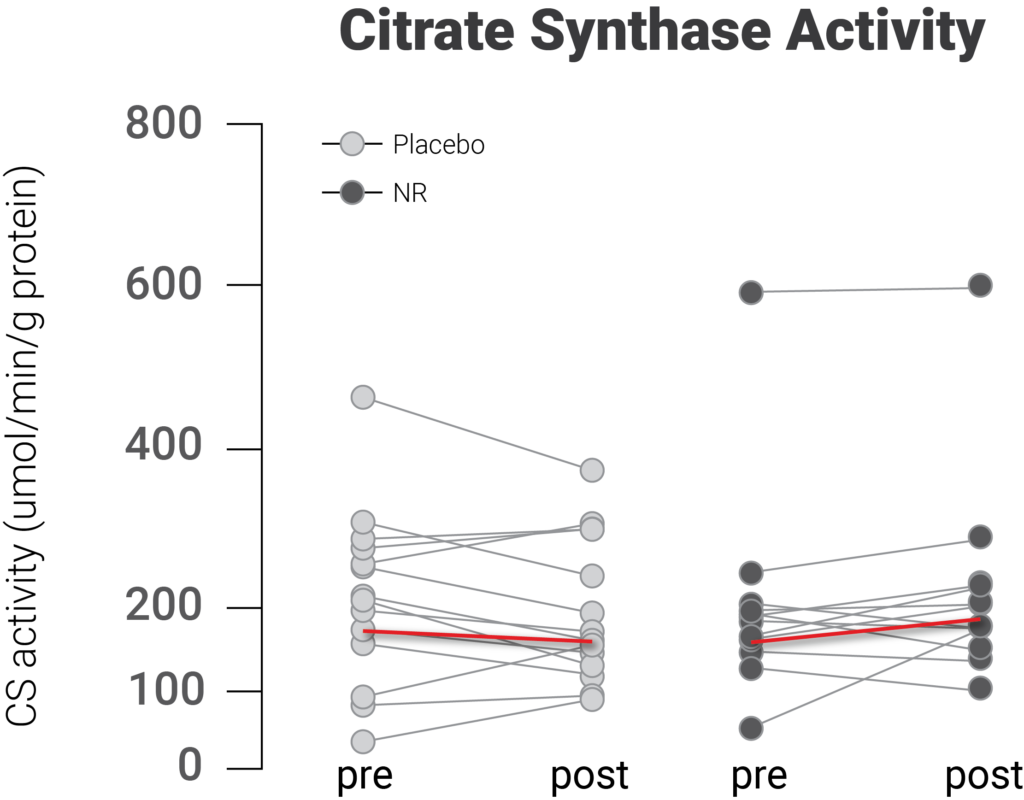
(Dollerup et al., 2020 | Journal of Physiology) NR supplementation did not increase mitochondrial abundance in human skeletal muscle. Activity levels of citrate synthase, indicative of mitochondrial abundance, did not increase in human skeletal muscle with NR supplementation.
The researchers then looked at whether supplementing with NR increases reactions that use oxygen for cellular energy production (i.e., respiration) and found NR did not improve this process in skeletal muscle. They didn’t find any differences when they used a respirometer, a device that measures oxygen exchange, to measure respiration after NR supplementation. “Following 12 weeks of supplementation, NR treatment did not improve the overall mitochondrial oxidative capacity in human skeletal muscle,” stated the scientists in their publication.
“Our data do not support the hypothesis that dietary NR supplementation has significant impact on skeletal muscle mitochondria in obese and insulin-resistant men. Future studies on the effects of NR on human skeletal muscle may include both sexes and potentially provide comparisons between young and older people,” stated the team. Future studies could also look at the effects of NR supplementation on cellular NAD+ content and mitochondrial function in age-related conditions other than obesity and insulin resistance.