Key Points:
- Older adults tend to nap longer and more frequently with aging.
- Longer and more frequent naps may be indicative of an increased the risk for Alzheimer’s dementia.
- Napping duration is also associated with lower cognitive performance in old age.
Does napping too much cause our wakefulness neurons to die, or do dead neurons cause us to nap excessively? In other words: which came first, the dead neurons or the excessive napping?
In an article published in Alzheimer’s & Dementia, in a collaboration between Harvard Medical School and the University of California San Francisco (UCSF), Li and colleagues addressed this chick-and-egg problem, showing that napping longer and more frequently increases the risk of Alzheimer’s disease in older adults. They also show that older adults nap more as they age and that excessive napping can lower cognitive performance.
“Daytime sleep behaviors of older adults are oftentimes ignored, and a consensus for daytime napping in clinical practice and health care is still lacking,” said Peng Li, the lead author of the study. “Our results not only suggest that excessive daytime napping may signal an elevated risk of Alzheimer’s dementia, but they also show that faster yearly increase in daytime napping may be a sign of deteriorating or unfavored clinical progression of the disease. Our study calls for a closer attention to 24-hour sleep patterns — not only nighttime sleep but also daytime sleep — for health monitoring in older adults.”
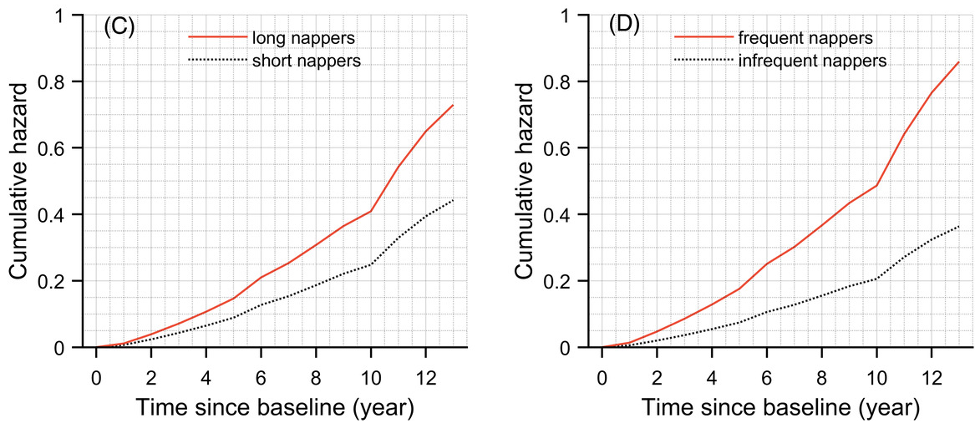
(Li et al., 2022 | Alzheimer’s & Dementia) Longer and More Frequent Naps Increase Risk for Alzheimer’s Disease. Plots show risk (cumulative hazard) for Alzheimer’s disease over 12 years in two representative individuals. (C) Napping ≥ 1 hour/day (long nappers) compared to ≤ 1 hour/day (short nappers) increases risk 1.4-fold. (D) Napping once or more a day (frequent nappers) compared to napping less than once a day (infrequent nappers) increases risk by 40%.
Objective Measurements to Untangle Link Between Napping and Alzheimer’s
Daytime napping and brain health are connected in a way that hasn’t been obvious. Older adults, especially those with Alzheimer’s disease, tend to nap excessively during the daytime. The proposed mechanism for excessive napping in Alzheimer’s disease patients is two-sided. On the one side, Alzheimer’s disease could interfere with neurons associated with wakefulness, promoting sleepiness. On the other side, excessive sleeping could lead to cognitive decline and Alzheimer’s disease.
Previous studies on the effect of napping on cognition have had mixed results. Some show that napping can improve mood and alertness, particularly in younger adults, while others show that excessive naps lead to poor cognition. Many of these studies have used self-reported assessments of napping, which are inherently subjective and, therefore, unreliable, especially for older adults with cognitive deficits. Additionally, all prior studies performed only a single nap assessment for each participant. It still hasn’t been clear whether napping habits change with aging and how this affects cognition.
Objective assessments of napping over many years are necessary to untangle the complex link between daytime napping and Alzheimer’s disease. “One of the unique settings of this study is that participants were followed annually with not only clinical assessments, but also motor activity monitoring that allowed objective measurement of daytime napping behavior,” said Li. “So-called ‘snoozes’ or periods of drowsiness are more likely to be detected by objective algorithm, but left out during self-report.”
Li and colleagues analyzed data from the ongoing Rush Memory and Aging Project (MAP) conducted at the Rush Alzheimer’s Disease Center in Chicago. There were 1,401 (76.5% female) participants with an average age of about 81. A device that looks like a watch called an Actical was used to monitor the movement of the participants. The Actical was worn for 14 days during each visit to the testing center each year. Napping was based on an algorithm incorporating wrist activity counts from the Actical device. Additionally, cognitive function was assessed annually with a battery of 21 neuropsychological tests. Mild cognitive impairment was judged based on these tests.
Napping Increases with Age
The statistical analysis of Li and colleagues revealed that nap duration and nap frequency were positively correlated with age. There were no differences between men and women, and education level had no effect. These findings show that older adults tend to increase how often they nap during the daytime with age. “Our hope is to draw more attention to daytime sleep patterns and the importance of patients noting if their sleep schedule is changing over time,” said co-senior author Kun Hu. “Sleep changes are critical in shaping the internal changes in the brain related to the circadian clocks, cognitive decline and the risk of dementia.”
Nap Time Accelerated In Alzheimer’s
Alzheimer’s disease is a progressive neurodegenerative disorder, meaning that the brain degenerates slowly over time. As more neurons are lost, cognitive ability – the capacity to remember, learn, and reason – declines until full-on Alzheimer’s disease is reached. Li and colleagues examined the effect of Alzheimer’s disease and mild cognitive impairment (a milder form Alzheimer’s disease) on nap duration and frequency in older adults. They found that mild cognitive impairment doubled nap duration and frequency. Moreover, Alzheimer’s disease sextupled nap duration and more than tripled nap frequency. These data suggest that cognitive impairment and Alzheimer’s disease accelerate the duration and frequency of daytime napping in older adults.
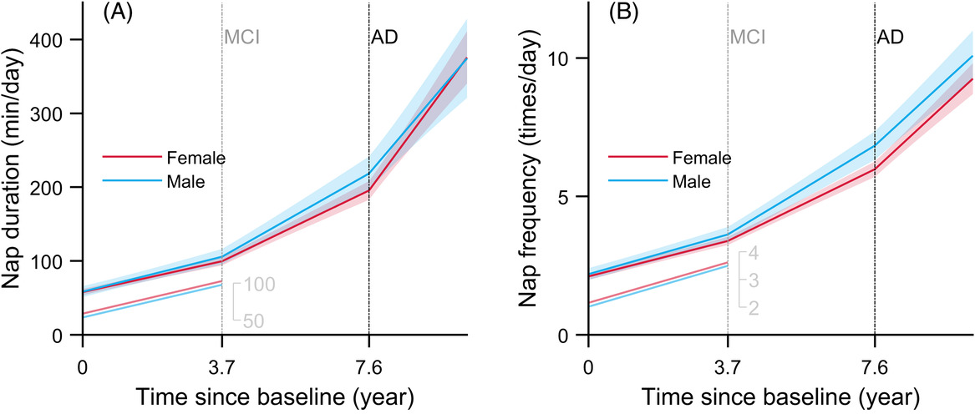
(Li et al., 2022 | Alzheimer’s & Dementia) Excessive Napping Accelerated by Mild Cognitive Impairment and Alzheimer’s. Plots show (A) nap duration and (B) frequency over time in older individuals. Individuals who developed mild cognitive impairment (MCI) after 3.7 years and Alzheimer’s disease after 7.6 years had an accelerated increase in both daytime nap duration and frequency.
Excessive Napping Associated with Higher Alzheimer’s Disease Risk
Li and colleagues next analyzed the association between daytime napping and the incidence of Alzheimer’s disease. A longer daytime nap was associated with a higher risk of developing Alzheimer’s disease, corresponding to a 1.6-year increase in age. More frequent naps were also associated with a higher risk of incident Alzheimer’s disease, with a 1.9-year increase in age. However, it is still unclear whether daytime napping and Alzheimer’s disease or cognitive decline are causally related.
“I don’t think we have enough evidence to draw conclusions about a causal relationship, that it’s the napping itself that caused cognitive aging, but excessive daytime napping might be a signal of accelerated aging or cognitive aging process,” said Yue Leng, the other co-senior author. “ It would be very interesting for future studies to explore whether the intervention of naps may help slow down age-related cognitive decline.”
Excessive Napping Is Linked to Decreased Cognitive Performance
Li and colleagues also determined how daytime napping and cognition drive each other’s changes over time using statistical models. The models demonstrated a decline in cognition over time. Cognition and nap duration were negatively correlated, meaning that individuals with faster cognitive decline tended to have increased nap duration over time. However, this association was not observed for nap frequency. This analysis suggests that napping for too long can lead to decreased cognitive performance as an older adult.
Nap Less?
This is the first study to demonstrate a bidirectional link between objectively measured napping and Alzheimer’s disease or cognitive impairment. Because the study results are based on correlations, whether excessive napping leads to cognitive impairment and Alzheimer’s disease or vice versa cannot definitively be extrapolated, but this is a good start, as other variables were also accounted for. “Importantly, these associations were independent from depressive symptoms, vascular diseases, and risk factors, and prescribed medications that may all contribute to sleep,” Li said.
Nighttime sleep disturbances were also accounted for in the analysis, implying that increased daytime napping was not to compensate for nighttime sleep loss. However, not all variables could be accounted for, and it is possible that daytime napping reflects poorer health in older individuals. Until this is all worked out, it might be best not to nap excessively during the daytime in old age.