Key Points:
- Nearly 42% of adults developed dementia after midlife, with women and Black adults facing the highest risks.
- 59% of carriers of the APOE ε4 gene developed dementia, significantly higher than the 39% incidence for non-carriers.
- Annual dementia cases in the U.S. are projected to double by 2060.
As lifespans increase, so does the shadow of dementia, a condition that strips away memories and cognitive function, affecting millions worldwide. Once considered an inevitable consequence of aging, dementia is now recognized as a pressing public health challenge with far-reaching social and economic implications. In a new study published in Nature Medicine, researchers provide updated estimates on the lifetime risk of dementia and project the future burden of the disease in the United States. Their findings reveal that nearly 42% of adults will develop dementia after midlife, highlighting the urgent need for preventive strategies and policy interventions.
Nearly Half of Women and Black Adults Face Elevated Dementia Risk
To provide contemporary insights into dementia risk, researchers analyzed data from the Atherosclerosis Risk in Communities (ARIC) study, which tracked over 15,000 adults across four diverse U.S. regions. Participants, who were dementia-free at the study’s baseline age of 55, were monitored over a median follow-up period of 23 years. The researchers employed cognitive assessments, telephone interviews, and medical record reviews to diagnose dementia cases and applied statistical models to estimate lifetime risk while accounting for mortality as a competing event.
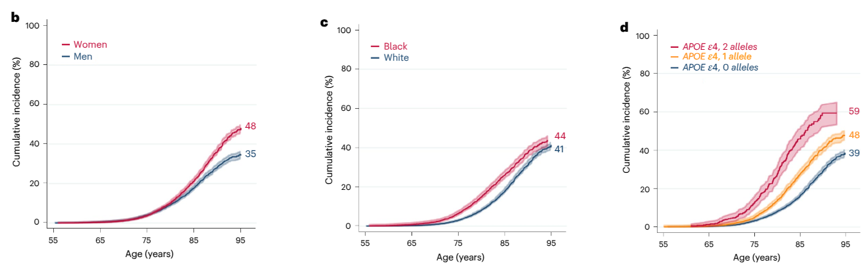
The study found that by the age of 95, 42% of participants developed dementia, with the risk varying significantly based on sex, race, and genetic predisposition. Investigators found that women had a markedly greater likelihood of developing dementia, with nearly 48% projected to develop dementia compared to 35% of men.
The data also revealed racial disparities, with 44% of Black adults developing dementia compared to 41% of White adults. Notably, genetic analysis indicated that individuals carrying the apolipoprotein E4 (APOE ε4) gene, a well-established risk factor for Alzheimer’s disease, experienced the highest incidence. Accordingly, participants with two copies of the gene had a dementia incidence of 59%, compared to 39% for those without the gene.
Lifestyle and Health Inequities Drive Rising Dementia Rates
The study’s projections indicate a nearly twofold increase in dementia cases over the next four decades, with annual cases expected to rise from 514,000 in 2020 to approximately one million by 2060. Additionally, the study points to several factors contributing to this increase, including the aging population, lifestyle-related health conditions such as obesity and hypertension, and the underdiagnosis of dementia in minority communities.
The findings also suggest that systemic inequities, such as disparities in healthcare access and socioeconomic status, may contribute to the higher dementia risk observed in Black adults. Moreover, evidence suggests that these populations often experience barriers to early diagnosis and intervention, leading to more advanced disease stages by the time of detection.
Strategies to Reduce Dementia Risk and Promote Healthy Aging
Although genetic predisposition plays a significant role in dementia risk, the study emphasizes the importance of modifiable lifestyle factors. Researchers estimate that addressing key risk factors—such as physical inactivity, poor diet, and untreated hearing loss—could prevent up to forty percent of dementia cases. Maintaining cardiovascular health through regular resistance training and blood pressure management, engaging in cognitively stimulating activities like chess, and adopting a heart-healthy diet rich in fruits, vegetables, and whole grains have all been linked to improved cognitive outcomes.
Despite the potential benefits of these interventions, only a small proportion of adults meet recommended health targets. With that said, public health initiatives that promote brain-healthy behaviors and provide accessible resources for early screening could help mitigate the growing burden of dementia.
Advances in Research Offer New Hope for Dementia Prevention and Treatment
The study’s findings underscore the need for continued investment in dementia research and healthcare innovation. Recent advancements in artificial intelligence and wearable health devices are improving early detection, while novel therapeutics targeting amyloid and tau proteins—the hallmarks of Alzheimer’s disease—are currently in development. Scientists believe that precision medicine approaches, which tailor interventions based on an individual’s genetic profile and lifestyle factors, may offer new opportunities to delay disease onset and improve quality of life.
Confronting the Dementia Epidemic
The findings from this large-scale study highlight the pressing need for comprehensive public health strategies aimed at reducing dementia risk and supporting affected individuals. Policy efforts should prioritize equitable healthcare access, targeted prevention programs, and increased funding for dementia research. While clinical trials for new treatments may take years to yield results, adopting preventive measures today remains the most effective strategy to combat the rising tide of dementia cases.
As the number of dementia cases continues to climb, individuals and healthcare systems must work together to promote cognitive health and ensure better outcomes for future generations.