Key Points:
- Electrically stimulating a critical nerve in mice enhances the resolution (stopping/ending) of inflammation, an underlying feature of aging.
- The resolution of inflammation is mediated by increases in the production of molecules derived from omega-3 fatty acids called pro-resolving lipids.
- This study has wider implications for the use of nerve stimulation therapy as a potential preventative measure against the many age-related diseases associated with chronic inflammation.
Our nervous system mediates all of our actions, including how we move, think, and feel. It also mediates unconscious (autonomic) processes like our heart rate, digestion, and immune system. The vagus nerve is the primary nerve associated with the unconscious “rest and digest” processes of the nervous system (parasympathetic nervous system). Recent discoveries have revealed that the vagus nerve may play a key role in resolving inflammation. However, until now, this has not been demonstrated in living organisms.
In a research article published in PNAS, Caravaca and colleagues from the Karolinska Institute in Sweden report that vagus nerve stimulation (VNS) promotes the resolution of inflammation by metabolic pathways associated with the increased production of pro-resolving lipids derived from omega-3 fatty acids. This study has wider implications for the use of VNS therapy as a potential preventative measure against age-related diseases associated with chronic inflammation.
“Inflammation and its resolution plays a key role in a wide range of common diseases, including autoimmune diseases and cardiovascular diseases,” says senior author Peder Olofsson. “Our findings provide insights on how the nervous system can accelerate resolution of inflammation by activating defined signaling pathways.”
VNS Treatment Resolves Inflammation Faster
To study the effect of VNS on the resolution of inflammation in living organisms, Caravaca and colleagues subjected mice to VNS by surgically exposing their vagus nerve and stimulating it with an electrode. An inflammatory response was then induced in the mice by injecting them with yeast cell wall particles (zymosan). To measure the magnitude of the inflammatory response, the investigators then counted the number of neutrophils — a type of white blood cell that increases as part of the inflammatory response. VNS-treated mice had a 34% reduction in the inflammatory resolution interval — time taken for cells (neutrophils) to decrease by half. Additionally, VNS treatment led to a reduction in other common pro-inflammatory molecules. These results indicate the VNS treatment shortens the time it takes for the inflammatory response to resolve.
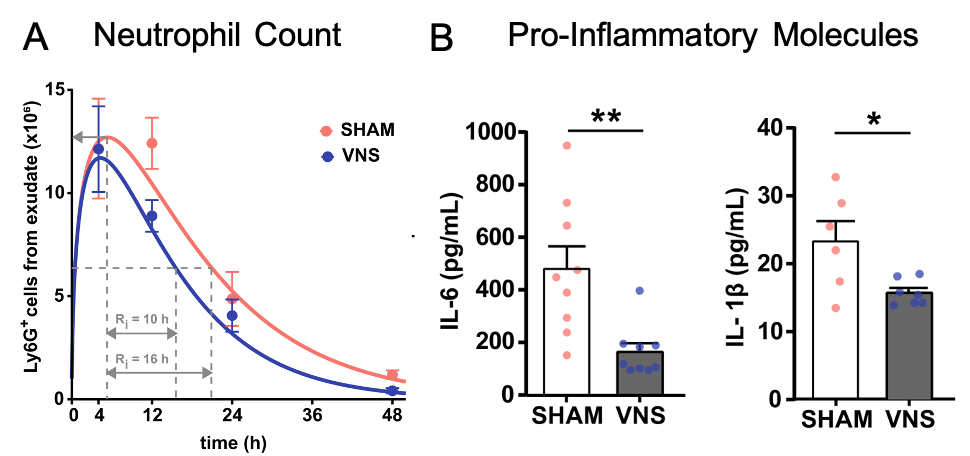
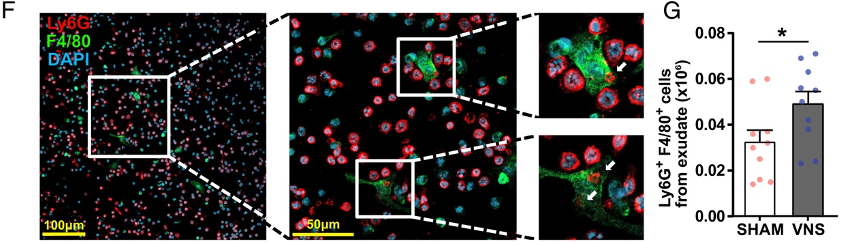
Inflammation is essential for defending against microbes and responding to tissue injury. However, the inflammatory response must eventually be resolved to avoid excessive tissue damage and disease. Only in the past two decades has this resolution of inflammation been discovered and investigated. A key process in the resolution of inflammation is the clearance of neutrophils by macrophages — a type of white blood cell that engulfs other cells for destruction. Thus, the resolution of inflammation can be measured by neutrophil clearance by macrophages.
To measure neutrophil clearance, Caravaca and colleagues imaged neutrophils and macrophages simultaneously in response to the induction of inflammation. They then counted the number of neutrophils engulfed by macrophages to view neutrophil clearance in action. They observed a higher number of neutrophils contained within macrophages in the mice treated with VNS, indicating increased clearance of neutrophils. These results show that VNS treatment regulates neutrophil clearance and inflammation resolution.
VNS Treatment Raises Production of Pro-Resolving Lipids
In 2004, the lipids that mediate the resolution of inflammation were discovered. These pro-resolving lipids (specialized lipid mediators) are derived from omega-3 and omega-6 polyunsaturated fatty acids. Pro-resolving lipids promote neutrophil clearance and counter proinflammatory molecules. Caravaca and colleagues found that pro-resolving lipids derived from omega-3s (DHA and n-3 DPA) were associated with VNS treatment. This, along with other changes in lipid mediators revealed that VNS shifted the balance of lipids to a more proresolving state.
“The vagus nerve is only one of many nerves that regulate the immune system. We will continue to map the networks of nerves that regulate inflammation at the molecular level and study how these signals are involved in disease development,” says Dr. Olofsson. “We hope that this research will provide a better understanding of how pathological inflammation can resolve, and contribute to more effective treatments of the many inflammatory diseases, such as atherosclerosis and rheumatism.”
Treating Chronic Inflammation with Vagus Nerve Stimulation
When inflammation is not resolved, it leads to chronic inflammation, which underlies many age-related diseases, including rheumatoid arthritis, cardiovascular disease, Alzheimer’s disease, and type 2 diabetes. Several clinical trials utilizing synthetic analogues of pro-resolving lipids are already underway for examining diseases like asthma, inflammatory bowel disease, and cardiovascular diseases. Therefore, by increasing the production of pro-resolving lipids, VNS could potentially be used to treat these diseases as well.
Whether VNS can be used to prevent or treat age-related chronic inflammation needs further investigation. Carvaca and colleagues examined the resolution of inflammation using a commonly used model, whereby acute inflammation is induced in the abdominal wall of mice, causing fluid to be excreted. The cells within this fluid are then measured over time to examine the resolution of inflammation. Thus, the model is limited to one tissue. Further studies will be needed to determine whether the model applies to other organs and tissues, especially those associated with common diseases, like the heart and brain. Studies examining the effect of VNS on chronic, rather than acute inflammation also seem necessary.
While not approved specifically for chronic inflammation, surgically implantable vagus nerve stimulators have been approved by the FDA for the treatment of epilepsy and depression. One non-invasive device has FDA approval for the treatment of cluster headaches. This device is called gammaCore and a 3 months supply can be purchased for $450 ($150/month). Another device called tVNS L that has approval in Europe for the treatment of epilepsy, depression, and pain runs for about 3,000 euros. In the future, when more evidence has accumulated, it is possible that these devices are approved for the treatment of diseases related to chronic inflammation.
