Key Points:
- Melatonin may counteract brain degeneration by staving off several biological drivers of aging, including inflammation.
- Melatonin has been shown to improve cognition in healthy subjects and individuals with mild AD.
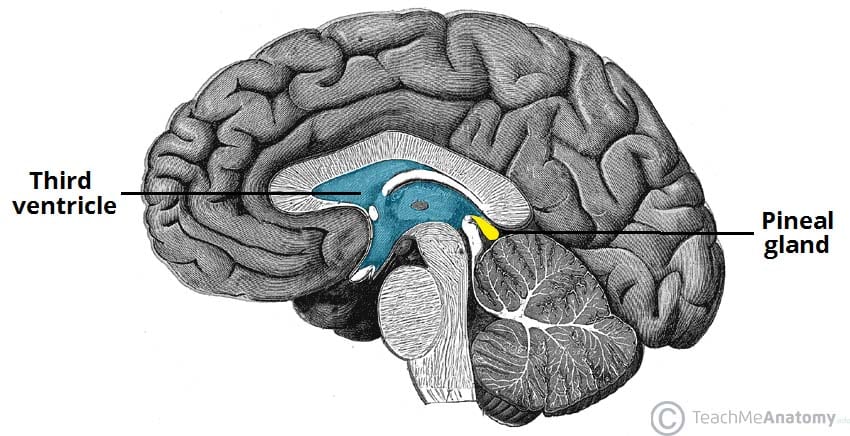
Aging is an insidious process, during which disadvantageous alterations to our cells progressively accumulate. However, melatonin — a hormone primarily secreted from a structure in the brain called the pineal gland — may potentially counteract these disease-triggering alterations.
Possibly due to the calcification of the pineal gland, melatonin levels gradually decline with age. The French philosopher René Descartes called the pineal gland “the seat of the soul,” as it is located in the center of the brain. The gland is also referred to as a third eye, especially in an ancient reptilian order known as the Rhynchocephalia, and some modern reptiles, as it has a similar structure to an eye. The human pineal gland still harbors the evolutionary remnants of this third eye in the form of photoreceptors — the cells in our eye that detect light and allow us to see.
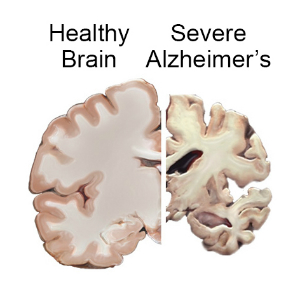
Like dysregulated melatonin, Alzheimer’s disease (AD) — a brain aging disease — is linked to poor sleep. AD patients have only 20% of the melatonin of non-AD patients. Moreover, a large dose of melatonin (100 mg/kg/day) has been shown to prolong the lifespan of mice that model AD. It follows that low melatonin levels could contribute to brain degeneration and accelerated aging.
How Melatonin Counteracts Brain Aging
Aside from improving sleep quality, preclinical studies have shown that melatonin is capable of counteracting several features of brain aging. Melatonin reduces the formation of beta-amyloid, an aberrant protein that accumulates in the brain and forms plaques. Beta-amyloid levels can predict both cognitive impairment and dementia and is a hallmark of AD.
Melatonin is also a potent antioxidant, meaning it neutralizes reactive oxygen species (ROS). Excessive ROS cause cellular damage called oxidative stress, a key biological driver of cellular aging. Prolonged oxidative stress induces neuron death, contributing to neurodegeneration, characterized by the loss of neurons.
In addition to counteracting oxidative stress, melatonin may mitigate inflammation, another biological driver of aging. The hormone may do so by placing the brain’s resident immune cells into an anti-inflammatory state, thereby counteracting neuroinflammation. Melatonin may also shield against neuroinflammation by safeguarding the blood-brain barrier, the deterioration of which could allow pro-inflammatory factors to enter the brain.
Melatonin Improves Cognition
Melatonin has been shown to improve cognition (e.g., learning and memory) in multiple AD mouse models. In humans, a meta-analysis of 22 studies showed that melatonin supplementation improved cognition in individuals with mild AD. Moreover, another meta-analysis of 50 studies and about 20,000 AD patients showed that melatonin was associated with improved cognitive function.
As for healthy subjects, a 2004 study showed that 1 mg of nightly melatonin for four weeks improved cognition (i.e., verbal learning). Additionally, a 2009 study showed that acute (one hour after taking) 3 mg of melatonin improved memory in young men under stress. In older healthy adults, a 2024 study suggested that melatonin protects against the atrophy of the hippocampus — the brain structure that consolidates memories.
Is Taking a Melatonin Supplement a Good Idea for All?
Prominent influencers, such as Stanford neuroscientist Andrew Huberman, PhD, have advocated against supplementing with melatonin. This is largely because melatonin is a powerful hormone and the doses found in supplements vary widely, sometimes not matching the label. Moreover, the dosage regimen needed to reap the cognitive benefits of melatonin has not been established. However, melatonin is safe and relatively inexpensive, making it an attractive anti-aging supplement.
Because it is difficult to assess brain health in the United States without expensive procedures, observing the early biological stages of cognitive decline and dementia is a challenge. Still, a good indicator of susceptibility to accelerated brain aging may be our sleeping patterns. If our sleep-wake cycles are irregular and our sleep quality seems poor (e.g., we still feel tired upon waking), melatonin supplementation could help with getting back on track. However, one should consult a healthcare provider before taking any supplements.