Key Points:
- Rats treated with NAD+ following a heart attack and cardiopulmonary resuscitation (CPR) have better survival outcomes and decreased neurological deficits.
- NAD+ treatment leads to better cardiac function following revival as compared to no treatment.
- NAD+ may facilitate better cardiac and neurological outcomes through its effects on mitochondrial function and sirtuins — longevity-associated enzymes.
As we age, our bodies are more susceptible to heart attacks and other instances of irregular heart rhythms. Cardiopulmonary resuscitation (CPR) is the standard of care following a heart attack. However, heart attack-induced oxygen deprivation can often lead to long-term cardiovascular and neurological issues that can lead to death. Now, researchers have found that nicotinamide adenine dinucleotide (NAD+) may prevent the medical concerns that often follow resuscitation from heart attacks via CPR.
Scientists from medical universities in China and Virginia published a study in Critical Care Medicine focused on rats treated with NAD+ following induced heart attacks. The scientists found that treating rats with NAD+ improved multiple measures of heart function, neurological deficits, and survival rates as compared to the untreated group. Furthermore, NAD+ treatment helped maintain mitochondrial function – the ability of the cell’s powerhouse (mitochondria) to generate cellular energy – which may be the mechanism behind NAD+’s effects on heart attack outcomes.
“These findings offer significant insight into developing new strategies for the treatment of post-resuscitation myocardial and neurologic dysfunction,” the scientists wrote.
NAD+ Treatment for Post-Heart Attack Recovery
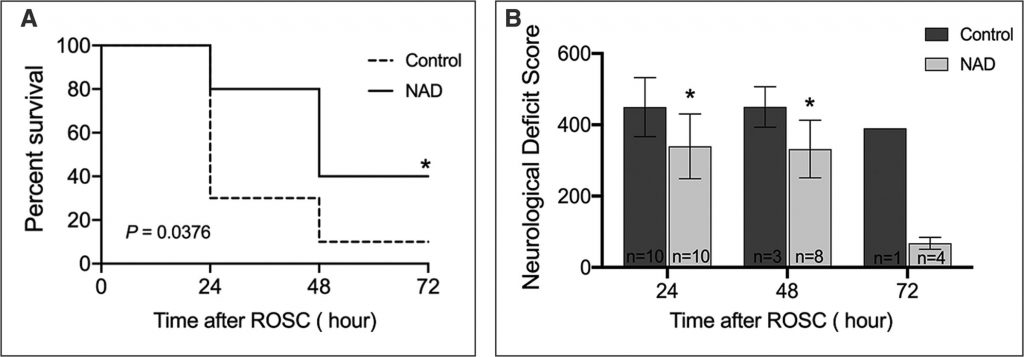
Su and colleagues used electrical wires to induce heart attacks (or irregular heartbeats) in rats. Following CPR, 90% (9/10) of the untreated rats died within the first 72 hours, as compared to 60% (6/10) of the NAD+-treated rats. Furthermore, early mortality – within the first 24 hours – was lower in the NAD+-treated group (2/10) as compared to the untreated group (7/10). Overall, NAD+ increased the survival rate of rats resuscitated via CPR.
The researchers also found significantly lower neurological deficits seen in the NAD+ group as compared to the untreated group. This was measured using a Neurological Deficit Scale (NDS), patterned after clinical evaluations of humans. The score was based on several behavioral tests, including tests of coordination, balance, reflexes, and anxiety.
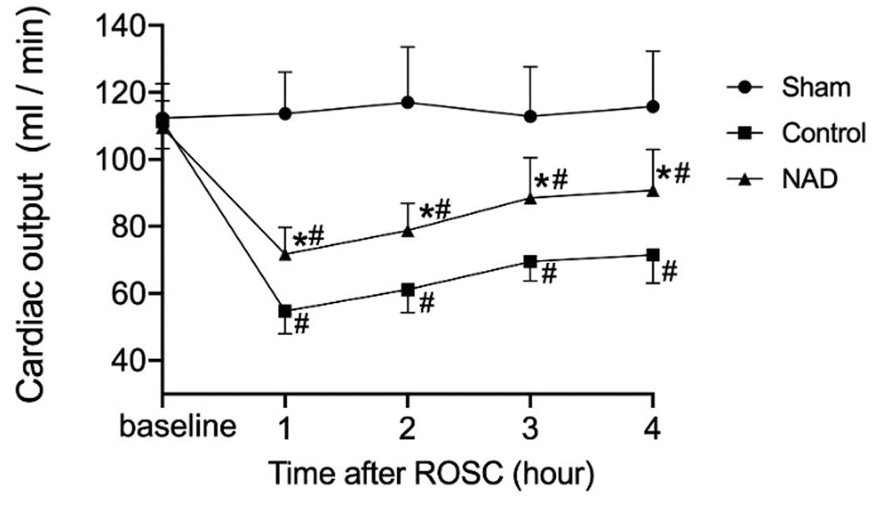
NAD+ treatment also helped to maintain cardiac function following heart attack with increased average blood pressure in the arteries, increased percentage of blood leaving the heart after each contraction, as well as increased cardiac output (the amount of blood pumped by the heart in a minute) as compared to the untreated rats in the four hours following the return of spontaneous circulation (ROSC) – the restoration of a regular heart rhythm that can sustain blood flow throughout the body following a heart attack.
Mitochondrial dysfunction is thought to play an important role in post-resuscitation heart and neurological conditions. NAD+-dependent enzymes (sirtuins), known to play a role in regulating mitochondrial energy production, protect the heart and brain against oxygen-deprivation injuries when activated. Su and colleagues found that treating rats with NAD+ helped restore mitochondrial energy production and energy molecule levels following heart attack by activating a specific sirtuin, Sirtuin3.
Is NAD+ An Option for Treating Post-Heart Attack Conditions?
Su and colleagues show here that NAD+ helps to reduce the effects of heart attacks on cardiac and neurological function. Other studies have shown that NAD+ has positive effects when it comes to protecting against irregular heart rhythms in mice and the inflammatory response seen in heart failure, further suggesting the role NAD+ may have in cardiac protection.
Furthermore, studies have also focused on NAD+’s role in maintaining heart health as we age, citing its protective effects on metabolism and heart failure. However, other studies have indicated the myriad of factors that can affect the aging heart, indicating the need for more research before we can consider NAD+ as a necessary therapy following a heart attack or its use as an anti-aging therapy for our hearts. As with any readily available supplement, speak to your doctor before starting or stopping any medications or supplements.